
Babesiosis in Canines
Babesia spp blood parasites are transmitted by ixodid ticks.
Babesia canis is a protozoan parasite that causes canine babesiosis, a tick-borne disease that can lead to life-threatening anemia and systemic illness in dogs. Found in many parts of the world, especially in tropical and subtropical regions, Babesia canis poses a significant health concern for both domestic and working dogs. This blog provides a comprehensive overview of the disease, covering its etiology, clinical signs, pathology, diagnosis, and treatment.
Etiology
Babesia canis is a large, intraerythrocytic protozoan parasite belonging to the phylum Apicomplexa. These include B canis, B vogeli, and B rossi. Babesia canis is transmitted by Dermacentor reticularis and Rhipicephalus ssp. in Pakistan. Babesia canis is transmitted by Dermacentor reticularis in Europe, B vogeli by Rhipicephalus sanguineus in tropical and subtropical countries, and B rossi by Haemaphysalis elliptica in South Africa. Consequences of Babesia infection vary from a mild, transient illness to acute disease that rapidly results in death. Transmission can also occur through blood transfusions, dog fights, or transplacentally, although tick bites remain the most common route.
There are three recognized subspecies:
-
B. canis vogeli – least pathogenic, found worldwide.
-
B. canis rossi – most pathogenic, found in sub-Saharan Africa.
-
B. canis canis – moderately pathogenic, common in Europe and Asia.
Pathology
Once inside the host, Babesia organisms invade red blood cells (RBCs), replicate asexually, and eventually cause their destruction. This leads to:
-
Intravascular hemolysis
-
Anemia
-
Hypoxia
-
Organ dysfunction
Severe infections may result in:
-
Splenomegaly
-
Hepatomegaly
-
Hemoglobinuria
-
Disseminated intravascular coagulation (DIC)
-
Multi-organ failure
Clinical Signs
The clinical presentation can vary depending on the virulence of the subspecies, immune status of the host, and level of parasitemia. Common signs include:
-
Lethargy
-
Fever
-
Anorexia
-
Pale mucous membranes
-
Jaundice (icterus)
-
Dark-colored urine (hemoglobinuria)
-
Splenomegaly
-
Tachycardia and tachypnea
-
Weight loss
-
In severe cases: collapse, neurologic signs, or death
Chronic infections may be subclinical but can flare under stress or immunosuppression.
Diagnosis
Diagnosis relies on a combination of clinical suspicion, laboratory testing, and diagnostic imaging:
-
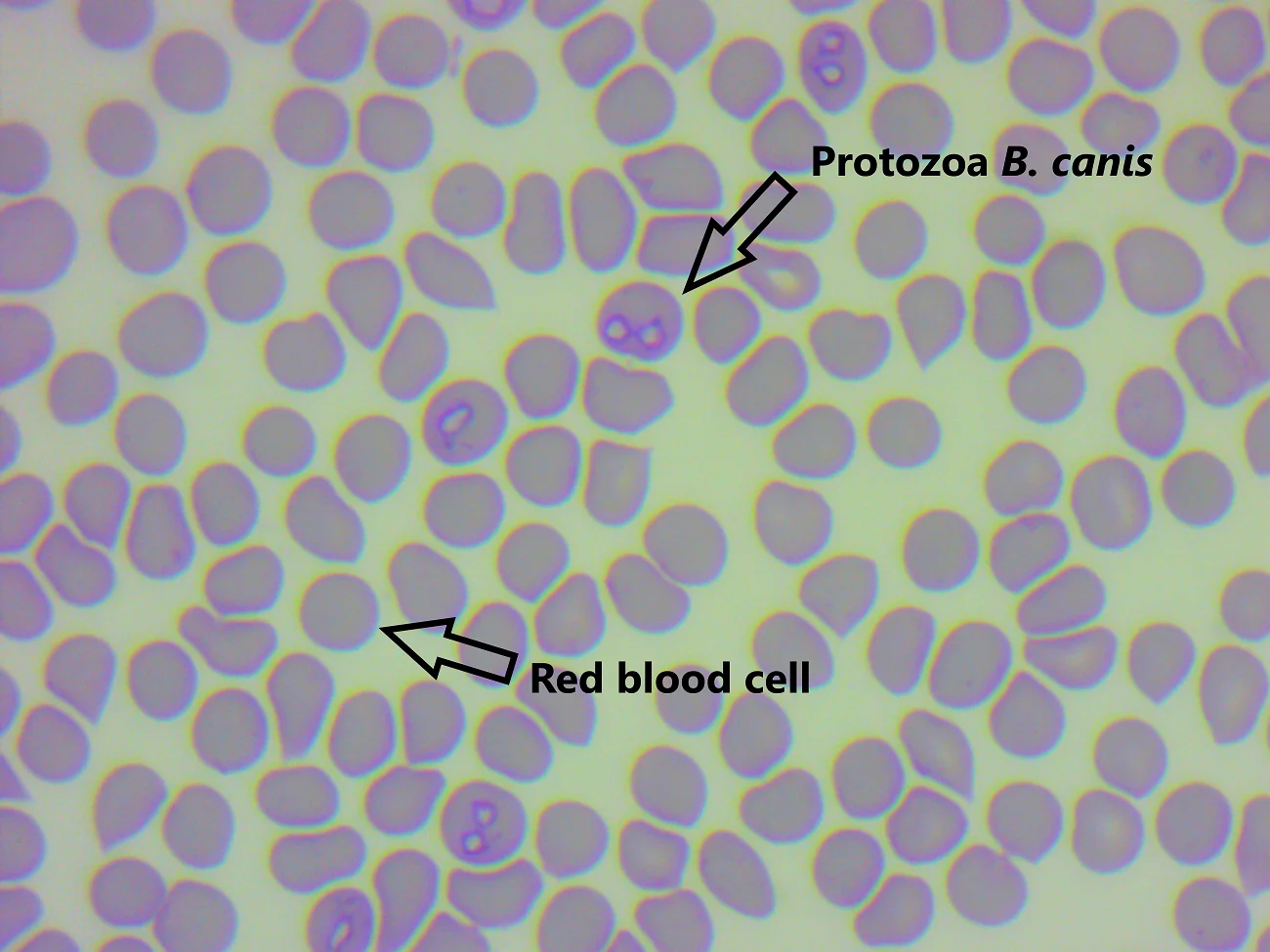
Blood Smear: Identification of piroplasms inside RBCs using Giemsa stain.
-
Complete Blood Count (CBC): Reveals anemia, thrombocytopenia, and leukocytosis.
-
Serology: Indirect fluorescent antibody test (IFAT) detects antibodies.
-
PCR Testing: Highly sensitive and specific, allows for subspecies identification.
-
Coagulation Profile: To evaluate for DIC in severe cases.
-
Biochemistry Panel: To assess liver and kidney involvement.
Treatment
Treatment of Babesia canis aims at eliminating the parasite and managing clinical symptoms.
Antiprotozoal Therapy:
-
Imidocarb dipropionate (5–6 mg/kg IM or SC) – most commonly used drug.
-
May require repeated dosing.
-
Monitor for side effects: pain at injection site, cholinergic signs (vomiting, salivation).
Supportive Therapy:
-
IV fluids for hydration and shock.
-
Blood transfusions in cases of severe anemia.
-
Antipyretics to manage fever.
-
Oxygen therapy if hypoxia is present.
Adjunctive Therapy:
-
Corticosteroids may be used in immune-mediated hemolysis (controversial).
-
Antibiotics (e.g., doxycycline) if concurrent infections are suspected (e.g., Ehrlichia).
Prevention
-
Tick control: Regular use of tick preventatives (acaricides, collars, spot-ons).
-
Avoid dog fights or situations with potential for blood contact.
-
Screen blood donors for Babesia prior to transfusion.
-
Vaccination: In some countries, vaccines (e.g., for B. canis) are available but offer partial protection.
Conclusion
Babesia canis infection can range from mild to severe, even fatal, especially in naïve or immunocompromised dogs. Prompt diagnosis and effective treatment are critical to a positive outcome. Veterinarians and pet owners must work together to maintain tick control and monitor for any signs of illness in at-risk dogs.
Regular veterinary checkups, proper tick prevention, and quick action at the first sign of symptoms can make a significant difference in managing this dangerous parasitic disease.
 |
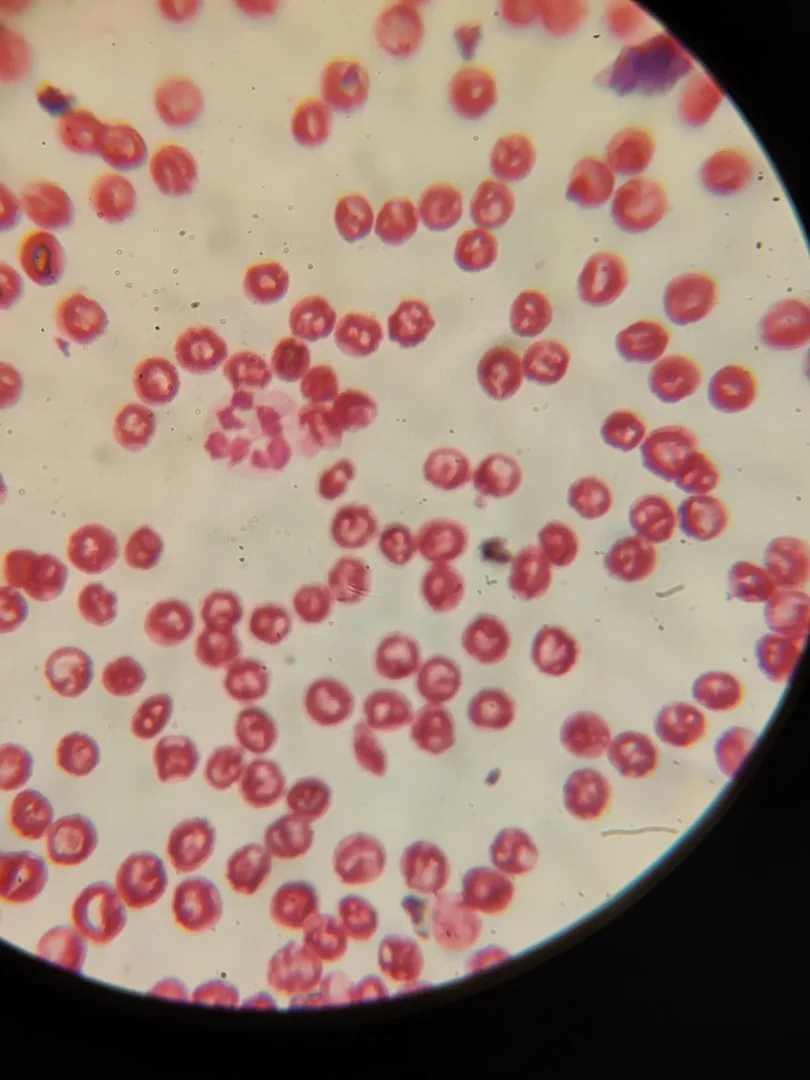 |
Case Description :
A three years old male GSD was presented at the hospital with the complaint of fever, lethargy, hemoglobinuria and sudden collapse. On physical examination the dog was found with sever tick infestation ( blacklegged tick) and Pale gums. CBC and blood smear shows severe anemia and and was diagnosed with Babesia canis via blood smear. Treatment included imidocarb dipropionate (5–6 mg/kg SC), IV fluids, iron supplements and tick control. The dog recovered fully within two weeks, with no parasites detected.
