
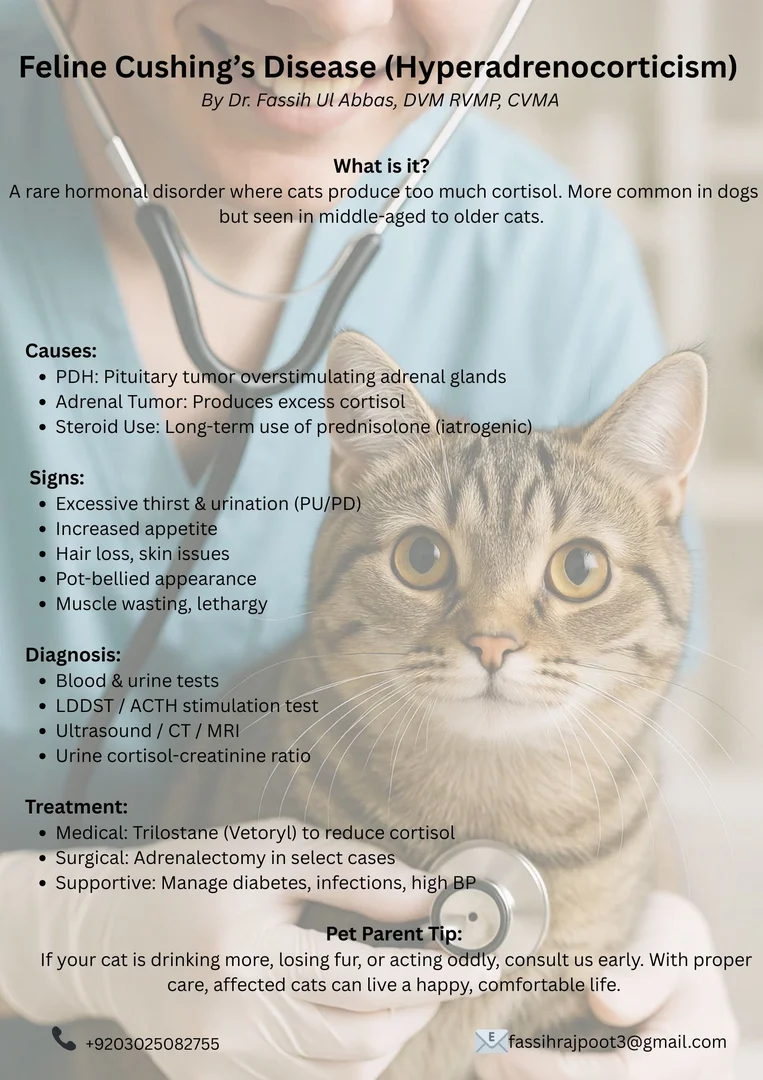
Feline Hyperadrenocorticism (Feline Cushing's Disease)
Understanding Feline Hyperadrenocorticism (Cushing’s Disease): A Guide for Pet Parents By Dr. Fassih Ul Abbas, DVM RVMP, CVMA
Introduction:
Feline hyperadrenocorticism, also known as Cushing’s disease, is a rare but serious hormonal disorder in cats. It occurs when the body produces excessive amounts of cortisol—a hormone essential for metabolism, stress response, and immune function. While more common in dogs, this condition can still affect felines, especially middle-aged to older cats. A unique feature of feline Cushing syndrome is severe thinning of the skin, which is susceptible to tearing (referred to as feline fragile skin syndrome).
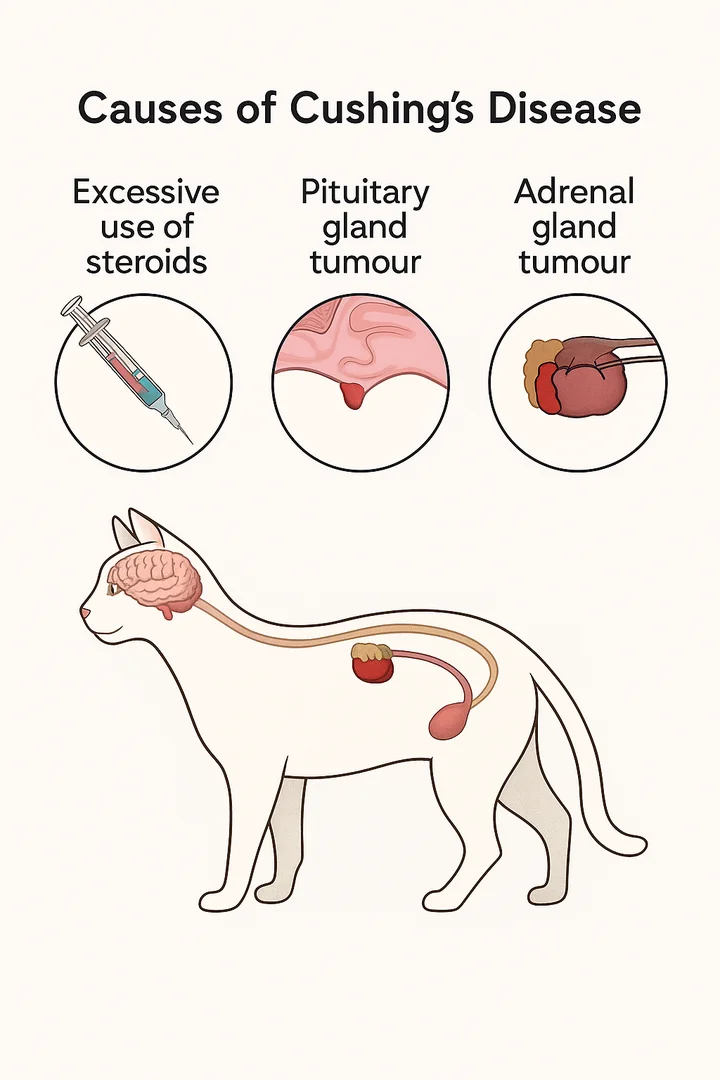
What Causes Hyperadrenocorticism in Cats?
The disease is usually caused by:
-
Pituitary-dependent hyperadrenocorticism (PDH): A small tumor in the pituitary gland overstimulates the adrenal glands.
-
Adrenal tumors: A growth on one of the adrenal glands that produces excess cortisol.
-
Iatrogenic Cushing’s: Long-term or high-dose steroid use (like prednisolone) can mimic this condition.
Clinical Signs to Watch For
Cushing’s disease develops gradually, making early signs easy to miss. Some common symptoms include:
-
Increased thirst and urination (PU/PD)
-
Increased appetite
-
Thinning of the skin
-
Muscle wasting and a pot-bellied appearance
-
Hair loss or poor coat condition
-
Lethargy or weakness
-
Diabetes mellitus (in some cases)
-
Recurring skin infections or delayed wound healing
Note: Many of these signs can overlap with other diseases like diabetes or kidney disease, which is why proper diagnosis is essential.
How Is It Diagnosed?
Diagnosing feline Cushing’s disease can be complex and often requires multiple tests:
-
Physical examination and history
-
Bloodwork and urinalysis – May show high liver enzymes, dilute urine, or signs of diabetes.
-
Low-dose dexamethasone suppression test (LDDST) – A key diagnostic tool that evaluates cortisol regulation.
-
ACTH stimulation test
-
Ultrasound or advanced imaging (CT/MRI) – Helps visualize adrenal or pituitary tumors.
-
Urine cortisol-to-creatinine ratio – A screening test but not very specific.
Treatment Options
Treatment depends on the type and severity of the disease:
-
Medical Management:
-
Trilostane (Vetoryl) is the most commonly used drug to control cortisol production.Medical treatment with trilostane is the mainstay of HAC treatment in cats, with a recommended dosing of ~1 mg/kg given two to three times daily with food.
-
Regular monitoring is essential to avoid under- or over-treatment.
-
Surgical Management:
-
If caused by an adrenal tumor, surgical removal of the affected gland (adrenalectomy) may be curative.
-
Surgery carries risks, especially in older or diabetic cats, and should be done by a veterinary surgical specialist.
-
Managing Secondary Conditions:
-
Diabetes, skin infections, and high blood pressure may require additional medications.
Prognosis
The outlook for cats with Cushing’s disease varies:
-
With proper management, many cats can enjoy a good quality of life.
-
Cats treated medically may require lifelong therapy and monitoring.
-
Surgical removal of adrenal tumors can be curative, but it depends on the tumor’s nature (benign vs. malignant) and surgical success.
-
If left untreated, Cushing’s can significantly decrease lifespan and quality of life.
Takeaway for Pet Parents
Although rare, feline hyperadrenocorticism is a serious condition that requires prompt diagnosis and long-term care. If your cat is drinking more water than usual, losing fur, or showing signs of diabetes or unusual weight gain, consult your veterinarian. Early intervention and consistent management can help your feline friend live comfortably and happily.
If you have questions about your cat’s health or want to learn more about endocrine disorders in pets, feel free to reach out through our online consultancy or visit our blog for more pet health tips
🐾 Case Study:
Feline Cushing’s Disease in a Rescue Cat
Patient: Brownie
Age/Sex: 6-year-old spayed female
Breed: Domestic Shorthair
History: Rescue cat with a 3-month history of polyuria/polydipsia (PU/PD) and voracious appetite, now presenting with anorexia and lethargy for the past week.
 |
 |
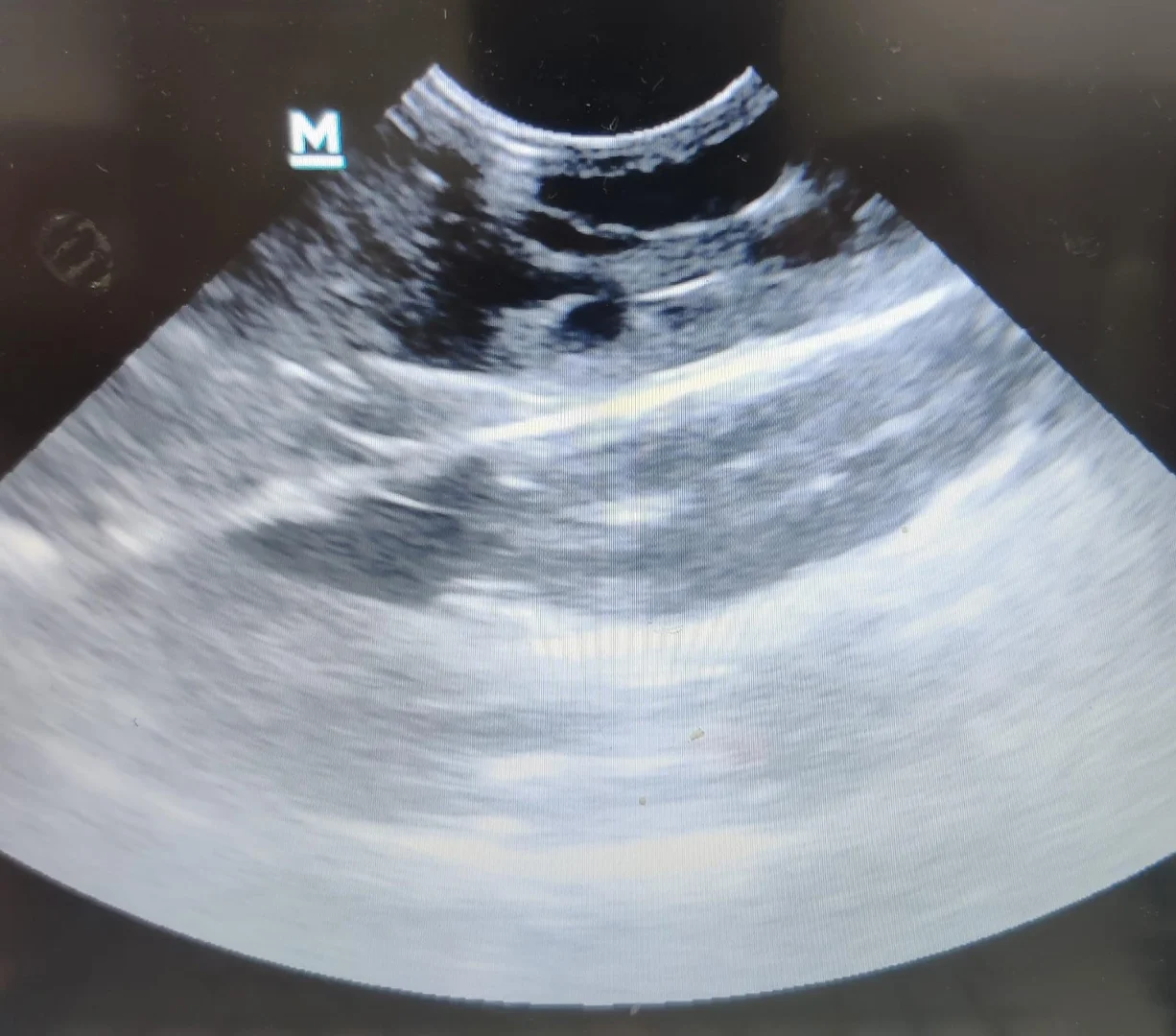
🩺 Clinical Findings
-
Physical exam: Muscle wasting, pot-bellied abdomen, thin skin with flank alopecia, Severe anemia, Flea infestation.
-
Vitals: Grade 4 Heart Murmurs.
-
Initial labs:
-
Mild hyperglycemia, elevated ALP, low USG
-
Negative for urinary tract infection
-
ACTH Stimulation Test: Elevated post-ACTH cortisol
-
Abdominal ultrasound: Bilateral adrenal enlargement, no adrenal mass.
 |
 |
✅ Diagnosis
Pituitary-Dependent Hyperadrenocorticism (Cushing’s Disease)
💊 Treatment & Outcome
Brownie was started on Trilostane and supportive care. Within two weeks, PU/PD decreased, appetite returned.
📌 Summary
This case highlights an atypical progression of feline Cushing’s where initial hyperphagia transitioned to anorexia as cortisol dysregulation advanced. Early endocrine testing in PU/PD cats with skin and behavioral changes is crucial for timely diagnosis and management.
